On October 6, we hosted the fourth webinar in our 2021 Virtual Chordoma Community Conference (CCC) Series, focused on improving balance, strength, and mobility after chordoma treatment. According to our Chordoma Survivorship Survey, roughly one-third of chordoma patients and survivors experience balance impairment, and 20 percent experience loss of mobility in their extremities. Chordoma patients and survivors with tumors at all locations along the spine report experiencing a range of mobility challenges, including loss of function in arms, hands, legs, or feet to vision impairment to the ability to walk or move around freely.
Understanding what causes these issues and knowing how to talk to your doctor about getting the right care are critical to improving physical functioning and overall quality of life. During this one-hour webinar, Lisa Ruppert, MD, a physiatrist and cancer rehabilitation expert at Memorial Sloan Kettering Cancer Center, and Justin Brown, MD, a reconstructive neurosurgeon at Massachusetts General Hospital’s Paralysis Center talked about the causes and symptoms of mobility issues in chordoma and how to manage them.
5 Key takeaways
1. A trained physiatrist can help coordinate your rehabilitative care
If your mobility has been affected by chordoma, there are ways to address the issues you’re experiencing. Speak to the doctors and nurses treating your chordoma about your symptoms and about connecting with a physical medicine and rehabilitation (PM&R) physician, also known as a physiatrist, to help coordinate your rehabilitative care. After an initial evaluation and consultation with your chordoma team, your physiatrist can help assemble a team of specialists to address your specific needs. This team may include oncologists, surgeons, physical therapists, occupational therapists, certified prosthetist orthotists (CPOs), assistive technology professionals (ATPs), or neuro-ophthalmologists, among others. It’s important to share medical records across all members of your team and ensure they talk to one another about your case.
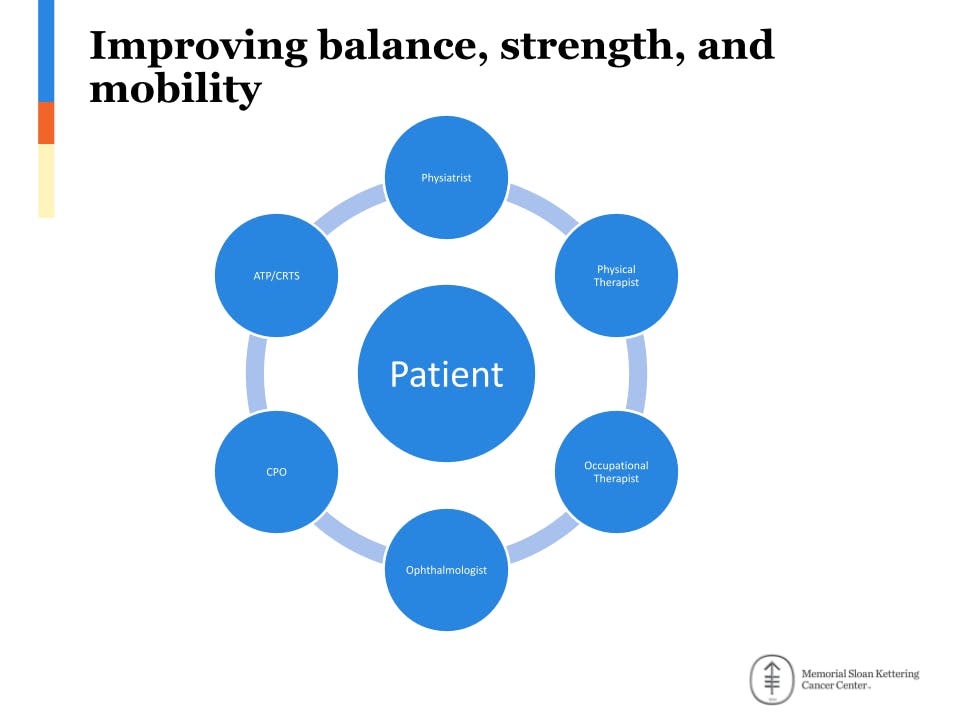
Slide from Dr. Ruppert's presentation
2. Having an individualized plan is crucial to meeting your mobility goals
There is no one-size-fits-all approach to regaining balance, strength, and mobility after chordoma treatment. Every patient needs an individualized plan. That plan begins with a comprehensive physical evaluation to assess your medical history, prior and current functional status, cognition, and pain level, as well as your personal goals for mobility and lifestyle. Once you and your care team are on the same page about your shared goals, they can help you build a long-term plan for managing and improving your mobility. This plan will likely include a combination of specialized therapy (like physical, occupational, or vision therapy), assistive devices (like wheelchairs, walkers, or braces), and at-home exercises.
3. Even if you traveled for your chordoma treatments, you may still be able to find rehabilitative specialists near home
Not every patient will have access to a physiatrist in their home region, and some may find that they need to assemble their own local care team. Professional associations such as the American Academy of Physical Medicine and Rehabilitation and the American Physical Therapy Association, your local academic medical center, and spinal cord support resources such as facingdisability.com and axisproject.org are all great places to start researching local specialists. Remember that while experience with chordoma is critical for your chordoma treatment, it is less important when dealing with side effects. Providers with experience treating your symptoms, along with a willingness to learn about chordoma and coordinate with your care team, will be able to provide you with the right care.
4. The field of reconstructive neurosurgery offers several surgical options for repairing damaged nerves, but many people aren’t aware of them
A number of reconstructive neurosurgical procedures developed for individuals with traumatic injury have been successfully used to improve mobility issues caused by chordoma and its treatments. These include nerve transfers to restore lost function in arms, hands, legs, or feet and procedures addressing spasticity or spinal cord compression paralysis. Surgical solutions for mobility issues caused by skull base and mobile spine chordomas are currently more advanced than those that address issues caused by sacral chordomas (such as bowel and bladder impairment) but these are on the horizon. But no matter where your tumor is/was located, if you are experiencing mobility issues, talk with your doctor about whether surgery can help. Besides Dr. Brown’s Paralysis Center at Massachusetts General, other centers around the U.S. have reconstructive neurosurgery experts.
5. It never hurts to ask
If you notice issues with your balance, strength, and mobility — even if you’re not sure they were caused by chordoma treatment or you don’t think there’s treatment for them — say something to your doctor. It’s better to ask the question and learn about your options than stay quiet and miss out on a solution that could help.
Educating providers on chordoma
Healthcare providers who can help you manage mobility issues might not know a lot about chordoma. And that’s okay. We developed a fact sheet you can use to help these doctors and providers learn about chordoma. It includes general information on chordoma, how it’s treated, and the common side effects of those treatments. There is also space for you to add information about your particular situation so your providers can understand how chordoma has affected you personally.
Watch the Webinar
Contact a Chordoma Foundation Patient Navigator
Chordoma Foundation Patient Navigators provide personalized information and support to anyone affected by chordoma, anywhere in the world, at any stage of their journey. Your Patient Navigator will use their extensive knowledge of chordoma to help answer your questions, provide information about treatment guidelines, help you find qualified doctors, talk with you about side effects, and connect you with others in the chordoma community who have been through a similar journey.